A collaborative project with Georgia CTSA's biostatistics program & Emory Renal Medicine faculty drastically cuts infection in hemodialysis patients
Georgia CTSA's Biostatistics, Epidemiology, & Research Design (BERD) program collaborated on a quality improvement project to decrease catheter-related infections in hemodialysis patients led by Vandana Dua Niyyar, MD, associate professor of medicine, Emory University School of Medicine, Ibironke Apata, MD, assistant professor of Medicine, Emory University School of Medicine, and James Bailey, MD, professor of medicine, Emory University School of Medicine.
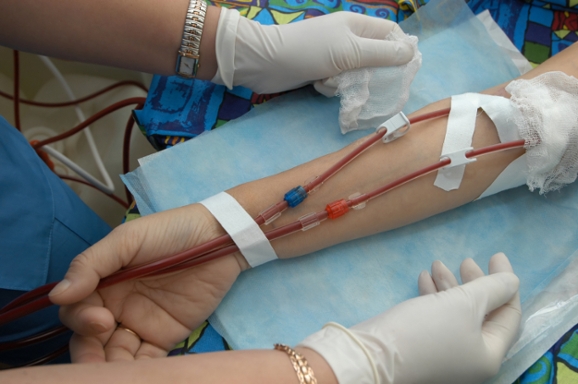
Hemodialysis is a treatment that replaces kidney function by filtering waste, removing extra fluid, and balancing electrolytes. During the treatment, blood is removed from the body and filtered through a man-made membrane called a dialyzer, or artificial kidney, and then the filtered blood is returned to the body. There are three ways to access the blood for hemodialysis, including AVF (arteriovenous fistulae); AVG (arteriovenous grafts) and central venous catheters (CVC). Of these, CVC are associated with increased infection rates, morbidity, and mortality.
Chlorhexidine-impregnated transparent (CHG-transparent) dressings allow for continuous antimicrobial exposure and easy visibility of the CVC insertion site. The research team conducted a quality improvement project to compare catheter-related infection (CRI) rates in two dressing regimens – CHG-transparent dressings and adhesive dry gauze dressing in hemodialysis patients with tunneled CVCs.
The study was conducted in two phases at three hemodialysis units. CRI rates at each hemodialysis unit during the 12-month intervention were compared to CRI rates for the 12-month pre-intervention period for each study phase. CRI rates were also compared between all three hemodialysis units. The study results, Chlorhexidine-impregnated transparent dressings decrease catheter-related infections in hemodialysis patients: a quality improvement project published in the Journal of Vascular Access, demonstrated that replacing adhesive dry gauze dressing with CHG-transparent dressing for hemodialysis patients with tunneled CVC was associated with decreased CRI rates.
BERD biostatistician and study co-author John Hanfelt, PhD, professor of biostatistics and bioinformatics, Rollins School of Public Health, Emory University and Director, BERD, discussed variables, performed statistical analysis of the catheter infection rates, reviewed data and analysis, and edited manuscript and presentations with the research team.
A key goal of the BERD program is to provide value-added assistance to markedly improve the quality of the translational and clinical research of Emory, Georgia Institute of Technology (Georgia Tech), Morehouse School of Medicine (MSM), and University of Georgia (UGA) investigators. This is accomplished by having highly trained, service oriented BERD personnel from Emory’s Rollins School of Public Health available to assist researchers in a timely manner.
The Georgia Clinical & Translational Science Alliance (Georgia CTSA) is a statewide partnership between Emory, MSM, Georgia Tech, and UGA and is one of over 60 in a national consortium striving to improve the way biomedical research is conducted across the country. The consortium, funded through the National Center for Advancing Translational Sciences (NCATS) and the National Institutes of Health’s Clinical and Translational Science Awards, shares a common vision to translate laboratory discoveries into treatments for patients, engage communities in clinical research efforts, and train the next generation of clinical investigators.