Georgia CTSA-supported Finding: an 'Achilles' heel' for the 'Iraqibacter'
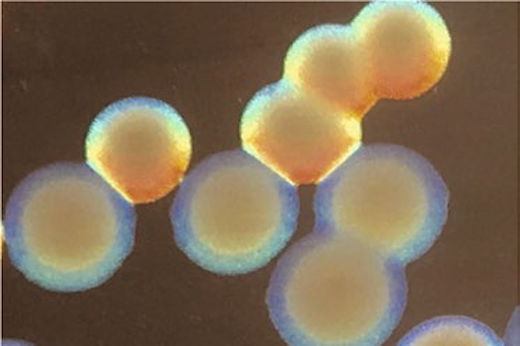
Colonies of ABaumannii
Emory University microbiologists have found an “Achilles’ heel” for Acinetobacter baumannii, a type of disease-causing bacteria. Acinetobacter baumannii is known as “Iraqibacter,” because it is found in soldiers returning from Iraq or Afghanistan in soft tissue infections. However, this was named one of the World Health Organization’s top three multidrug resistant threats in 2017 and is “notoriously difficult to fight with disinfectants or detergents as well as antibiotics. A. baumannii is most commonly seen in ventilator-association pneumonia or central-line-associated blood stream infections.”
The microbiologists found a genetic switch which makes it possible to “switch” between a virulent, hardy form and an avirulent form. Once the bacteria is in its avirulent form, the bacteria becomes more vulnerable to host defense molecules and disinfectants. Co-author Phil Rather, PhD, professor, Department of Microbiology and Immunology, Emory University says, “This switch could be an Achilles’ heel for Acinetobacter…it could be the key for small molecules that could lock it in the avirulent state.” The researchers further showed that a strain of the bacteria that was artificially engineered to be locked in the avirulent state, could induce a protective immune response and successfully vaccinate mice against Acinetobacter infection. In addition, “there are other components to the virulence switch.” The next step according to Rather is to study “other genes that affect the switch.”
The study was done in collaboration with David Weiss, PhD, associate professor, director of the Emory Antibiotic Resistance Center, and in part by the Robert P. Apkarian Integrated Electron Microscopy Core. The Integrated Electron Microscopy Core is subsidized by the Emory College of Arts and Sciences and the Emory University School of Medicine and is one of the Emory Integrated Core Facilities.
To support the rapid evaluation and translation of high-impact emerging technologies, the Georgia CTSA’s Innovation Catalyst program established the Proof-of-Principle Fund. These funds, along with support from the Georgia Research Alliance (GRA), are used to invest in new, promising technologies, such as the Robert P. Apkarian Integrated Electron Microscopy Core, that are aligned with the Georgia CTSA strategic goals.
The Georgia Clinical & Translational Science Alliance (Georgia CTSA) is an inter-institutional magnet that concentrates basic, translational, and clinical research investigators, community clinicians, professional societies, and industry collaborators in dynamic clinical and translational research projects. Emory engaged three of its close academic partners – Morehouse School of Medicine, Georgia Institute of Technology, and the University of Georgia – to form the Georgia CTSA. This partnership, a strategic multi-institutional alliance, offers compelling, unique, and synergistic advantages to research and patients statewide.
Georgia CTSA is one of nearly 60 in a national consortium striving to improve the way biomedical research is conducted across the country. The consortium, funded through the National Center for Advancing Translational Sciences (NCATS) and the National Institutes of Health’s Clinical and Translational Science Awards, shares a common vision to translate laboratory discoveries into treatments for patients, engage communities in clinical research efforts, and train the next generation of clinical investigators.